Jurisdiction 1 Part BPulmonary Rehabilitation (PR) Services
MLN Matters® Number: MM6823 Revised
Related Change Request (CR) #: 6823
Related CR Release Date: May 7, 2010
Effective Date: January 1, 2010
Related CR Transmittal #: R124BP and R1966CP
Implementation Date: October 4, 2010
Note: This article was revised on July 10, 2012, to add clarifying language, as contained in Change Request (CR) 6823, to show that the covered benefit for the comprehensive Pulmonary Rehabilitation (PR) program is for patients with moderate to severe COPD. All other information is the same.
Provider Types Affected
This article is for physicians and providers submitting claims to Medicare Contractors (Medicare Administrative Contractors (A/B MACs), Fiscal Intermediaries (FIs) and/or Carriers) for pulmonary rehabilitation (PR) services provided to Medicare beneficiaries.
Provider Action Needed
This article is based on Change Request (CR) 6823 which alerts providers that the Medicare Improvements for Patients and Providers Act (MIPPA) of 2008 added payment and coverage improvements for patients with chronic obstructive pulmonary disease (COPD) and other conditions effective January 1, 2010. As a result, Medicare provides a covered benefit for a comprehensive PR program under Medicare Part B effective for services on or after January 1, 2010. As a result, Medicare provides a covered benefit for a comprehensive PR program for patients with moderate to very severe COPD under Medicare Part B effective for services on or after January 1, 2010. Be certain your billing staffs are aware of these Medicare changes and of the claims processing system changes to handle claims for PR services that must be implemented no later than October 4, 2010.
Background
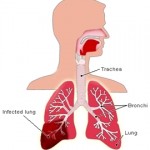
PR is a multi-disciplinary program of care for patients with chronic respiratory impairment who are symptomatic and often have decreased daily life activities.
A PR program is individually tailored and designed to optimize physical and social performance and autonomy. The program must provide an evidence-based, multidisciplinary, and comprehensive intervention for patients with chronic respiratory impairment. In September 2007, the Centers for Medicare & Medicaid Services (CMS), in its final decision memorandum for PR Services, announced there was no basis for a national coverage determination at that time. Specifically, this decision was based on a determination by CMS that the Social Security Act (The Act) did not expressly define a comprehensive PR program as a Part B benefit, and the evidence was not adequate to draw conclusions on the benefit of the individual components of PR. CMS did (and still does) cover medically reasonable and necessary respiratory treatment services in Comprehensive Outpatient Rehabilitation Facilities (CORFs), as well services to patients with respiratory impairments who are not eligible for PR but for whom local contractors determine respiratory treatment services are covered. MIPPA added payment and coverage improvements for patients with COPD and other conditions, and now provides a covered benefit for a comprehensive PR program for patients with moderate to very severe COPD under Medicare Part B effective January 1, 2010. This law authorizes a PR program, which was codified in the Physician Fee Schedule calendar year 2010 final rule at 42 CFR 410.47.
Key Points of CR 6823
Effective January 1, 2010, MIPPA provisions added a physician-supervised, comprehensive PR program for patients with moderate to very severe COPD. Medicare will pay for up to two one-hour sessions per day, for up to 36 lifetime sessions (in some cases, up to 72 lifetime sessions) of PR. The PR program must include the following mandatory components:
- Physician-prescribed exercise
- Education or training
- Psychosocial assessment
- Outcomes assessment
- An individualized treatment plan
The following bullet points detail Medicare claims processing requirements for PR services furnished on or after January 1, 2010:
- Effective January 1, 2010, Medicare Contractors will pay claims containing Healthcare Common procedure Coding System (HCPCS) code G0424 when billing for PR services, including exercise and monitoring, as described in the Medicare Benefit Policy Manual, Chapter 15, section 231, as revised by CR 6823, and the Medicare Claims Processing Manual, Chapter 32, Section 140, as revised by CR 6823. These revised documents are attached to CR 6823, which is available at http://www.cms.gov/Transmittals/downloads/R124BP.pdf (Benefit Policy Manual) and http://www.cms.gov/Transmittals/downloads/R1966CP.pdf (Claims Processing Manual) on the CMS website.
- Medicare Contractors will pay claims for HCPCS code G0424 (PR) only when services are provided in the following places of service (POS): 11 (physician’s office) or 22 (hospital outpatient). Medicare will deny claims for HCPCS code G0424 performed in other than, and billed without, POS 11 or 22, using the following:
- Claim Adjustment Reason Code (CARC) 58 – ‘treatment was deemed by the payer to have been rendered in an inappropriate or invalid place of service. NOTE: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.’
- Remittance Advice Remark Code (RARC) N428 – ‘Service/procedure not covered when performed in this place of service.’
- Group Code PR (Patient Responsibility) assigning financial liability to the patient if the claim was received with a GA modifier indicating a signed Advance Beneficiary Notice (ABN) is on file or Group Code CO (Contractual Obligation) assigning financial liability to the provider if the claim is received with the GZ HCPCS modifier indicating no signed ABN on file.
- Medicare Contractors will pay claims for PR services containing HCPCS code G0424 and revenue code 0948 on Types of Bill (TOB) 13X and 85X under reasonable cost.
- Contractors will pay for PR services for hospitals in Maryland under the jurisdiction of the Health Services Cost Review Commission on an outpatient basis, TOB 13X, in accordance with the terms of the Maryland waiver.
- Contractors will deny claims for PR services provided in other than TOB 13X and 85X using the following:
- CARC 58 – ‘Treatment was deemed by the payer to have been rendered in an inappropriate or invalid place of service. NOTE: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.’
- RARC N428 – ‘Service/procedure not covered when performed in this place of service’
- Group Code PR assigning financial liability to the patient if the claim was received with a GA modifier indicating a signed ABN is on file or Group Code CO assigning financial liability to the provider if the claim is received with the GZ HCPCS modifier indicating no signed ABN on file
- Using the Medicare Physician Fee Schedule, Medicare Contractors will also pay for PR services billed with HCPCS code G0424 and revenue code 096X, 097X or 098X on TOB 85X from Method II critical access hospitals (CAHs).
- Medicare will deny PR services that exceed two units on the same date of service and, in doing so, will use the following:
- CARC 119 – ‘Benefit maximum for this time period or occurrence has been reached’
- RARC N362 – ‘The number of days or units of service exceeds our acceptable maximum’
- Group Code PR assigning financial liability to the patient if the claim was received with a GA HCPCS modifier indicating a signed ABN is on file or Group Code CO assigning financial liability to the provider if the claim is received with the GZ HCPCS modifier indicating no signed ABN on file
- Medicare will normally pay for 36 sessions of PR, but may pay up to 72 sessions when the claims for sessions 37-72 includes a KX HCPCS modifier. Claims for HCPCS code G0424 which exceed 36 sessions without the KX HCPCS modifier will be denied using the following:
- CARC 151 – ‘Payment adjusted because the payer deems the information submitted does not support this many/frequency of services’
- Group Code PR assigning financial liability to the patient if the claim was received with a GA HCPCS modifier indicating a signed ABN is on file or Group Code CO assigning financial liability to the provider if the claim is received with the GZ HCPCS modifier indicating no signed ABN on file
- Medicare Contractors will deny claims for HCPCS code G0424 when submitted for more than 72 sessions even where the KX HCPCS modifier is present. In the denials, contractors will use the following:
- CARC B5 – ‘Coverage/program guidelines were not met or were exceeded’
- Group Code PR assigning financial liability to the patient if the claim was received with a GA HCPCS modifier indicating a signed ABN is on file or Group Code CO assigning financial liability to the provider if the claim is received with the GZ HCPCS modifier indicating no signed ABN on file
Additional Information
CR 6823 was issued to your Medicare MAC, FI or Carrier in two transmittals. One transmittal modifies the Medicare Benefit Policy Manual and that transmittal is available at http://www.cms.gov/Transmittals/downloads/R124BP.pdf on the CMS Web site. The second transmittal modifies the Medicare Claims Processing Manual and that transmittal is at http://www.cms.gov/Transmittals/downloads/R1966CP.pdf on the CMS Web site.
For related detailed policy and claims processing instructions issued December 11, 2009, you may review MM 6715 at http://www.cms.gov/MLNMattersArticles/downloads/MM6751.pdf on the CMS Web site.
Reprinted: http://www.palmettogba.com – 7/16/12.
Source: http://www.palmettogba.com.